Matt Lemieszewski
Rotation 1 – Internal Medicine
Identifying Data
January 19th, 2022 – 1:15PM
KM, 87F, Black, Widowed, Queens,NY
Informant: Patient, reliable
Referral Source: Self, daughter
Chief Complaint: Syncopal episode yesterday
History of Present Illness:
KM is an 87-year-old right-handed female with PMHx of HTN, HLD, DM, CAD s/p stents (last MI 8 years ago) on ASA 81mg QD, CVA (15 years ago) with no residual deficits, CKD, aortic stenosis, iron deficiency anemia, GERD, and PVD who presents from home after a syncopal episode yesterday afternoon around noon. Patient was recently told she needs an aortic valve replacement but needed her lab work to be improved prior to intervention. Patient has been receiving IV iron transfusions with her hematologist-oncologist once a week since 1/3/22. Per daughter, patient’s dizziness first started on 1/3/22 after the first IV iron treatment and has been persistent daily since. Had an appointment with heme-oncology scheduled on 1/18/22 for infusion but was cancelled due to patient’s complaint of dizziness. Patient came home from doctor’s office, ate lunch, and reportedly woke up on the floor at 8pm. Patient last recalls sitting on her couch at 1pm. Does not recall black-out and denies blurry vision, double vision, or lightheadedness prior to fall. Amount of time with loss of consciousness is unknown along with any possible head trauma. Patient’s daughter dropped her off at home at 12pm and daughter said the patient “was her normal self.” At 8pm patient was awoken by a phone call from her niece who stated the patient sounded “out of it” with “slurred words.” Daughter assumed patient’s symptoms were from being “exhausted.” At 11pm niece called again patient said she was in bed. At 7am (1/19/22) the patient’s niece went to her residence and found her in bed “weak and afraid to stand by herself and sweating.” Patient ambulated with 2-person assist into car and was taken to the hospital. Patient describes the dizziness as the room spinning sensation that is worse when she turns her head side to side and sits up. Patient also endorses a left ear infection 1 month ago treated with course of antibiotics. At the time of patient interview, patient states her dizziness has improved although still present if she sits up too quickly.
Past Medical History:
- Myocardial infarction
- Aortic stenosis
- CVA
- HTN
- HLD
- T2DM
- CKD
- Iron deficiency anemia
- GERD
- Hypercholesterolemia
Past Surgical History:
- Angioplasty with stent placement (2000, 2007, 2012)
Medications:
- Atorvastatin PO 40mg bedtime
- ASA 81mg PO QOD
- Carvedilol 25mg PO BID
- Hydralazine 50mg PO TID
- Sitagliptin 25mg PO QD
Allergies:
- NKA
Family History:
- Father: Deceased, CAD
- Mother: Deceased, unknown medical history
- Sister: Alive, CAD, T2DM,
Social History:
- Diet: Does not follow dietary regime
- COVID: Received 2 doses of Pfizer vaccine + booster (10/21)
- Home: Lives at home alone.
- Smoking: Denies ever smoking cigarettes or other tobacco products.
- Alcohol: Denies drinking any beer, wine, or liquor.
- Drugs: Denies use of any illicit drugs.
- Sleep: Sleeps 6-8hrs/night using 1 pillow. Denies use of a CPAP device
- Travel: Denies any recent travel
Review of Systems:
General: Admits generalized weakness and dizziness on movement. Denies any recent weight loss or gain, loss of appetite, night sweats, fever, or chills
Skin, hair, and nails: Denies changes in texture, excessive dryness or sweating, discolorations, pigmentations, moles/rashes, pruritus, or changes in hair distribution.
Head: Admits headaches, vertigo, and minimal nausea. Denies vomiting.
Eyes: Denies corrected vision, visual disturbances, double vision, blurriness, excess tearing or dryness, photophobia, or pruritis. Last eye exam over 10 years ago.
Ears: Admits ear infection one month ago. Denies hearing loss, tinnitus, discharge, earache.
Nose and sinuses: Denies discharge, obstruction, allergies, or epistaxis
Mouth and throat: Denies sore throat, bleeding gums, ulcerations. Does not wear dentures. Unknown last dental exam
Neck: Denies localized swelling, lumps, stiffness, or decreased range of motion.
Pulmonary: Denies shortness of breath, wheezing, or productive cough. Denies hemoptysis, cyanosis, orthopnea, or paroxysmal nocturnal dyspnea.
Cardiovascular: Denies chest pain, palpitations, edema, irregular rhythms.
Gastrointestinal: Denies changes in appetite, intolerance to any foods, no vomiting/dysphagia or pyrosis. No constipation or abdominal pain. Last colonoscopy 15 years ago.
Genitourinary: Denies incontinence, dysuria, nocturia, urgency, oliguria, or polyuria.
Nervous: Positive for headaches, and LOC. Denies seizures, sensory disturbances, ataxia, loss of strength, change in cognition/mental status/memory, or weakness
Musculoskeletal: Denies joint pain, swelling, weakness, changes in range of motion, or instability.
Peripheral Vascular: Denies peripheral edema, intermittent claudication, or varicose veins.
Hematologic: No history of DVT/PE. Positive history of iron transfusions.
Endocrine: Denies heat/cold intolerance, excessive sweating.
Psychiatric: Positive history of depression and anxiety. Denies having SI/HI or previously seeing a mental health professional.
Physical Exam:
General: 87F, A&O x2 (self, and place), lying in bed, gowned, well groomed, not in acute distress. She is not ill-appearing or diaphoretic.
Vitals:
- BP(Seated): R – 110/72
- P: 84bpm, regular (last EKG obtained in ED showing NSR)
- R: 14breaths/min, unlabored
- T: 98.8F (37.1C), oral
- O2 Sat: 97% RA
- Height: 66 inches – Weight: 119lbs – BMI: 19.2 Normal range
Skin: Warm and moist with good turgor throughout. Nonicteric. No erythema and warmth. Nontender on palpation. No jaundice.
Hair: Average quantity and distribution.
Nails: No clubbing, capillary refill <2 seconds in all four extremities
Head: Normocephalic, atraumatic, nontender to palpation throughout.
Eyes: Symmetrical OU. No strabismus, exophthalmos, sclera white, cornea clear, conjunctiva pink.
- Visual uncorrected – 20/30 OS, 20/40 OD, 20/40 OU
- Visual fields full OU. PERRLA, EOMs intact with no nystagmus
- Fundoscopy – Red reflex intact OU. Cup to disk ratio< 0.5 OU. No AV nicking, hemorrhages, or exudates
Ears: Symmetrical and appropriate in size. No masses, lesions, or deformities on external ears. No discharge or foreign bodies in external auditory canals AU. TM’s white and intact with light reflex in good position AU.
Mouth:
- Lips: Pink and moist with no lesions
- Mucosa: Pink with no masses or lesions. Non-tender to palpation. No leukoplakia.
- Palate: Intact with no masses or lesions Non-tender to palpation; continuity intact.
- Teeth: Good dentition with no obvious dental caries noted.
- Gingivae: Pink. No hyperplasia; masses; lesions; erythema or discharge.
- Tongue: Pink; well papillated with no masses or lesions. Non-tender to palpation.
- Oropharynx: Well hydrated, no masses, lesions, or foreign bodies. Grade 1 tonsils, class II Mallampati score. Uvula pink, no edema
Neck: Trachea midline. 2+ Carotid pulses, no stridor, thrills, or bruits noted bilaterally.
Thyroid: Nontender to palpation, no masses, no bruits noted. No thyromegaly.
Chest: Symmetrical, no deformities or trauma. Respirations unlabored, no paradoxical respirations or use of accessory muscles noted. Non-tender to palpation throughout.
Lungs: CTAB, normal chest expansion, positive breath sounds bilaterally, no wheezing, rales, or rhonchi.
Heart: Carotid pulses are 2+ bilaterally without bruits. RRR, S1 and S2 are distinct with no murmurs, S3 or S4. PMI in 5th ICS in mid-clavicular line.
Abdomen: Abdomen is symmetric without striae, no pulsations. Bowel sounds normoactive in all four quadrants with no aortic/renal/iliac/femoral bruits. Non-tender to palpation or percussion throughout. No guarding or rebound tenderness.
Peripheral Vascular: Skin normal in color and warm to touch upper and lower extremities bilaterally. No calf tenderness or edema bilaterally. Pulses are 2+ bilaterally in upper and lower extremities.
Musculoskeletal: No edema, erythema, soft tissue swelling, or tenderness present on bilateral upper and lower extremities. FROM of all upper and lower extremities bilaterally. No evidence of spinal deformities.
Neurologic:
- Mental Status: Alert and oriented to person and place only. Speech spontaneous, fluent, and prosodic without paraphasic errors. Naming and repetition intact. Follows complex commands.
- CN II-XII
- II: Visual fields full.
- III, IV, VI: EOMI, left gaze nystagmus, no gaze preference
- V: V1-V3 intact bilaterally
- VII: facial movement symmetric
- VIII: hearing intact to finger rub
- IX, X: no dysarthria, uvula midline, no aphasia
- XI: shoulder shrug 5/5 bilaterally
- XII: tongue midline
- Motor: Normal bulk and tone. No abnormal movements. No pronator drift, finger taps rapid and symmetric.
- Sensory: Intact to light touch and temperature in all four extremities.
- Coordination: No dysmetria on finger-nose-finger or heel-to-shin.
- Reflexes:
| R | L | R | L | ||
| Brachioradialis | 2+ | 2+ | Patellar | 2+ | 2+ |
| Triceps | 2+ | 2+ | Achilles | 2+ | 2+ |
| Biceps | 2+ | 2+ | Babinski | Absent | Absent |
| Abdominal | 2+/2+ | 2+/2+ | Clonus | Negative |
- Meningeal Signs: No nuchal rigidity noted. Brudzinski’s and Kernig’s signs negative
- NIHSS: NIH Stroke Scale
- Level of Consciousness (1a.): Alert, keenly responsive
- LOC Questions (1b.): Answers both questions correctly
- LOC Commands (1c.): Performs both tasks correctly
- Best Gaze (2.): Normal
- Visual (3.): No visual loss
- Facial Palsy (4.): Normal symmetrical movements
- Motor Arm, Left (5a.): No drift | Motor Arm, Right (5b.): No drift
- Motor Leg, Left (6a.): No drift | Motor Leg, Right (6b.): No drift
- Limb Ataxia (7.): Absent
- Sensory (8.): Normal, no sensory loss
- Best Language (9.): No aphasia
- Dysarthria (10.): Normal
- Extinction and Inattention (11.) (Formerly Neglect): No abnormality
- NIH Stroke Scale: 0
- GCS: Glasgow Coma Scale
- Eye Opening: Spontaneous
- Best Verbal Response: Oriented
- Best Motor Response: Obeys commands
- Glasgow Coma Scale Score: 15
- Modified Rankin (Modified Rankin Interval: Pre-stroke): Modified Rankin Score: 1
- No significant disability. Able to carry out all usual activities, despite some symptoms.
Initial labs/imaging:
- CT Head without IV contrast: small vessel ischemic changes. Otherwise, unremarkable examination.
- CXR 1-View (AP Only): No acute pulmonary disease
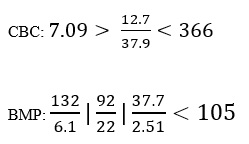
- Potassium sample severely hemolyzed, not accurate measure without repeat available.
Assessment: KM is an 87-year-old female with PMHx of CKD, HTN, DM, HLD, CVA with no residual deficits, CAD s/p stents on ASA 81mg, and GERD presenting from home after an unwitnessed fall/syncope yesterday and transient dizziness.
Differential Diagnosis:
- Benign Paroxysmal Positional Vertigo
- Transient Ischemic Attack
- Orthostatic Hypotension
- Ischemic Stroke
- Cranial mass/lesion
Plan:
#Dizziness and Unwitnessed Fall
- Admit to general medicine for syncope workup – low suspicion for acute stroke
- IVF 0.9% NS at 94mL/hr using 4-2-1 rule.
- Redraw BMP to see corrected electrolytes and treat accordingly
- Administer Meclizine 12.5mg TID for dizziness
- Administer Zofran 4mg PRN for any associated nausea
- Administer Lovenox 40mg SC QD
- Schedule TTE to evaluate aortic stenosis as possible etiology for syncope
- Consider cardiology consult
- Obtain orthostatic vitals
- Schedule MRI-brain
- Fall precautions
#HTN/HLD/T2DM
- Continue ASA, Lipitor, and Sitagliptin
Patient Education:
Mrs. M, our team has spoken with the attending doctor, and we wanted to let you know that you are being admitted because of your fall. You had your CT-scan done and though it does not appear that you have had a stroke, we would like to keep you here for a few days to try and understand why you passed out yesterday. We are going to keep you hydrated and draw some more labs while we run some tests to see if there may be another cause. We’ve spoken to your daughter, and she is on board with the plan. We’ll continue to make sure that you get all of your medications as well as something for the dizziness, but we want you to let us know if any of your symptoms get worse or feel like they did before you fell.


