Identifying Data
January 26th, 2022 – 6:00AM
CP, 37M, Hispanic, Queens, NY
Informant: Chart, ED staff
Referral Source: EMS
Chief Complaint: Found unconscious on sidewalk
History of Present Illness
CP is a 37-year-old male with PMH of ETOH abuse and history of multiple recent falls, latest 12 days ago and was admitted to Elmhurst Hospital with traumatic subdural hematoma, BIBEMS presented to the ED today after being found on the sidewalk with altered mental status. When patient was brought to ER, he was intoxicated, mumbling but moving all extremities with good strength. Patient was later brought to CT Head and after CT scan, the patient started to deteriorate, and patient was intubated in CEU. Neurosurgery was consulted after patient was intubated. CT head showed a large intraparenchymal hemorrhage and adjacent hemorrhages centered in the left temporal and posterior left frontal lobes, spanning a region of up to 9 cm, with surrounding edema. Mild subarachnoid hemorrhages in these regions as well with small subdural hematoma at the left temporal convexity overlying the left intracranial hematoma.
Past Medical History:
- Right subdural hematoma 1/2023 – received TXA and Keppra
- Interhemispheric fissure subarachnoid hemorrhage 6/2022 – received TXA and Keppra
Past Surgical History: Unknown
Medications: Started in hospital. Home medications unknown.
- Acetaminophen 975mg, Orogastric tube, Q6h
- Enoxaparin 40mg, SC, nightly
- Famotidine 20mg, orogastric tube, Q12h
- Levetiracetam (Keppra), 1,000mg, IV Q12h
- Propranolol 20mg, orogastric tube Q8h
- Thiamine 100mg, orogastric tube daily
- Lorazepam PRN
Allergies: Unknown
Family History: Unknown
Social History: +EtOH abuse, remainder unknown
Review of Systems: Unable to obtain due to intubation at the time of consult
Physical Exam:
General: 37M, patient intubated and sedated in CEU, unable to follow any commands, awaiting transport to OR
Vitals:
- BP(Seated): R – 131/78 [113/133]/[52-78]
- P: 70 [65-104]
- R: 14, ventilated
- T: 38.1C [37.8-38.5]
- O2 Sat: 100% ventilated [96-100]
- Height: 65 inches – Weight: 137.8lbs – BMI: 22.78 – Normal
General RASS score: 0
HEENT: Orally intubated, OGT in place, left pupil 4mm, sluggish, right pupil 2mm, sluggish
Cardiovascular: regular rate & rhythm
Respiratory: Ventilating via ETT
Abdomen: Soft, nondistended
GU: Foley in place with light yellow urine
Musculoskeletal: Moves left sided extremities purposefully to noxious stimuli. Minimal withdraw to RLE to noxious stimuli. No movement to RUE
Neuro: GCS E(1)V(NT)M(4)
Associated Imaging:
CT Head was done which showed a large IPH and adjacent hemorrhages centered in the left temporal and posterior left frontal lobes, overall spanning a region of up to 9 cm, with surrounding edema. Intramural hematoma anteriorly inferiorly in the right frontal lobe, overall spanning a region of approximately 2.8 cm, surrounding hematoma. Mild subarachnoid hemorrhages in these regions as well with small subdural hematoma at the left temporal convexity overlying the left intracranial hematoma.
Associated mass effect, including lateral shift of midline structures, medialization of the uncus, and findings suspicious for early/incipient herniation. Neurosurgery consulted for the above findings.
Labs:
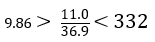
BMP:
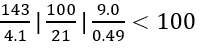
CBC:
T&S: O+
ABG
- pH 7.32
- PCO2 48
- HCO3 24.4
Prothrombin Time: 13.0 (10.0 – 13.0 seconds)
INR: 1.12 (0.87 – 1.13)
Ethanol Level: 294.2
- 50-100 mg/dL: Flushing, slowing of reflexes, impaired visual acuity
- > 100 mg/dL: Depression of CNS
- > 400 mg/dL: Fatalities reported
Assessment:
37M with history of EtOH abuse and several falls with TBI presented on 1/25/23 with intoxication and large left temporal IPH yielding midline shift and uncal herniation along with right IPH, L subdural hematoma, subarachnoid hemorrhage, required intubation and was taken to OR for left craniectomy and R EVD placement.
Plan
#TBI
- Book as Level 1 for left hemicraniectomy for decompression, possible ICH evacuation. Right frontal EVD placement.
- Repeat CT head 1/27
- HOB > 30 degrees
- Monitor ICP and CPP via EVD
- Monitor EVD outputs
- Continue Keppra 1g BID
#EtOH Abuse
- Continue Thiamine 100mg daily
- Monitor electrolyte abnormalities
#Hypertension
- Continue Propranolol
- Continue hemodynamic monitoring
#Acute blood loss anemia
- Trend hemoglobin, transfuse PRN
#DVT prophylaxis
- Lovenox 40mg injection SC nightly


