Matt Lemieszewski
Rotation 3 – Emergency Medicine
Identifying Data
March 29th, 2022 – 7:30PM
LB, 61M, African American, Queens, NY
Informant: Accompanying officers
Referral Source: Corrections Facility
Chief Complaint: Syncopal Episode
History of Present Illness:
LB is a 61-year-old male with a PMH of HTN, T2DM, DCMP, HFrEF (EF 27% 12/2021), BPH, bilateral inguinal hernias, pleural effusion, LV thrombus and DVT who presents from Rikers Correction Center via police escort after a witnessed syncopal episode today. As per correction officers at bedside, patient was in the court room and passed out. Officer explained that the patient stood up and fell over and was caught by another officer. Patient was helped to floor and did not hit his head. Length of time unconscious was about 30 seconds. Patient does not remember the incident and did not have any injuries or complaints on arrival. Patient reports that the jail gives him his medications daily, but he is unsure if he took them today. Patient presented to QHC on March 17th, 2022, for shortness of breath and chest pain and was admitted for 5 days for CHF exacerbation. At this time, patient denies previous syncopal episodes, chest pain, shortness of breath, dizziness, change/loss in vision, diaphoresis, abdominal pain, nausea, vomiting, fever, or chills.
Past Medical History:
- HTN
- T2DM
- Dilated cardiomyopathy
- HFrEF
- BPH
- DVT
- Pleural effusion
Past Surgical History:
- Bilateral hip arthroplasty – unknown date
Medications:
- Aspirin 81mg tablet, PO daily
- Atorvastatin (Lipitor) 40mg tablet, PO daily
- Carvedilol 12.5mg tablet, PO twice daily
- Empagliflozin (Jardiance) 10mg tablet, PO daily
- Entresto (Sacubitril/Valsartan) 49mg/51mg tablet, PO twice daily
- Furosemide (Lasix) 80mg tablet, PO twice daily
- Spironolactone 25mg tablet, PO daily
- Tamsulosin 0.4mg tablet, PO daily
Allergies:
- NKDA/NKFA
Family History: Family history limited as patient refusing to answer
Social History: Social history limited as patient refusing to answer
Review of Systems: ROS limited as patient refusing to answer
General: Denies any recent weight loss or gain, loss of appetite, generalized weakness or fatigue, night sweats, fever, or chills
Skin, hair, and nails: Denies changes in texture, excessive dryness or sweating, discolorations, pigmentations, moles/rashes, pruritus, or changes in hair distribution.
Head: Denies headaches, migraines, vertigo, nausea, or vomiting.
Eyes: Denies corrected vision. Denies visual disturbances, double vision, blurriness, excess tearing or dryness, photophobia, or pruritis. Last eye exam mm/yy
Ears: Denies hearing loss, tinnitus, vertigo, discharge, earache.
Nose and sinuses: Denies discharge, obstruction, or epistaxis
Mouth and throat: Denies sore throat. Denies bleeding gums, ulcerations. Does not wear dentures. Last dental exam mm/yy
Neck: Denies localized swelling, lumps, stiffness, or decreased range of motion.
Pulmonary: Denies shortness of breath. Denies cough, wheezing, hemoptysis, cyanosis, orthopnea, or paroxysmal nocturnal dyspnea.
Cardiovascular: Denies chest pain at rest or on exertion. Denies palpitations, edema, irregular rhythms.
Gastrointestinal: Has no change in bowel habits, with no changes in color or consistency. Denies changes in appetite, intolerance to any foods, no nausea/vomiting/dysphagia, pyrosis. No constipation, bleeding, (hemorrhoids, melena, or hematochezia), or abdominal pain. Last colonoscopy mm/yy
Genitourinary: Denies incontinence, dysuria, nocturia, urgency, oliguria, or polyuria.
Nervous: Positive loss of consciousness. Denies seizures, headache, sensory disturbances, ataxia, loss of strength, change in cognition/mental status/memory, or weakness.
Musculoskeletal: Denies any joint pain or swelling, weakness, or changes in range of motion.
Peripheral Vascular: Denies peripheral edema. Denies intermittent claudication.
Hematologic: Positive history of DVT. Denies previous blood transfusions.
Endocrine: Denies heat/cold intolerance, excessive sweating.
Psychiatric: Denies history of depression and anxiety. Denies having SI/HI or previously seeing a mental health professional.
Physical Exam:
General: 61M, A&O x3, lying on bed, legs restrained by handcuffs, speaking in full sentences, not in acute distress. Appears angry.
Vitals:
- BP(Seated): L – 184/112
- P: 71, regular
- R: 20breaths/min, unlabored
- T: 97.5F (36.4.C), oral
- O2 Sat: 99% on room air
- Height: 67 inches – Weight: 160lbs – BMI: 25.1 – Overweight.
Skin: Warm and moist with good turgor throughout. Nonicteric. No lower extremity erythema and warmth. Nontender on palpation. No cyanosis or jaundice.
Hair: Average quantity and distribution.
Nails: No clubbing, capillary refill <2 seconds in all four extremities
Head: Normocephalic, atraumatic.
Eyes: Symmetrical OU. No strabismus, exophthalmos, sclera white, cornea clear, conjunctiva pink.
- Visual uncorrected – 20/30 OS, 20/30 OD, 20/25 OU
- Visual fields full OU. PERRLA, EOMs intact with no nystagmus
- Fundoscopy – Red reflex intact OU. Cup to disk ratio< 0.5 OU. No AV nicking, hemorrhages, or exudates
Ears: Symmetrical and appropriate in size. No masses, lesions, or deformities on external ears. No discharge or foreign bodies in external auditory canals AU. TM’s white and intact with light reflex in good position AU.
Mouth:
- Lips: Pink and moist with no lesions
- Mucosa: Pink with no masses or lesions. Non-tender to palpation. No leukoplakia.
- Palate: Intact with no masses or lesions Non-tender to palpation; continuity intact.
- Teeth: Good dentition with no obvious dental caries noted.
- Gingivae: Pink. No hyperplasia; masses; lesions; erythema or discharge.
- Tongue: Pink; well papillated with no masses or lesions. Non-tender to palpation.
- Oropharynx: Well hydrated, no masses, lesions, or foreign bodies. Grade 1 tonsils, class II Mallampati score. Uvula pink, no edema
Neck: Trachea midline. 2+ Carotid pulses, no stridor, thrills, or bruits noted bilaterally.
Thyroid: Nontender to palpation, no masses, no bruits noted. No thyromegaly.
Chest: Symmetrical, no deformities or trauma. Respirations unlabored, no paradoxical respirations or use of accessory muscles noted. Non-tender to palpation throughout.
Lungs: No wheezing, rhonchi, or rales. Chest expansion and diaphragmatic excursion symmetrical.
Heart: Carotid pulses are 2+ bilaterally without bruits. RRR, S1 and S2 are distinct with no murmurs, S3 or S4.
Abdomen: Covered by blanket, patient refused exam.
Neurologic:
- Mental Status: Alert and oriented to person, place, and time. Affect is angry. Behavior is agitated and aggressive.
- CN II-XII grossly intact.
- Motor/Cerebellar: Full active/passive ROM in all extremities without rigidity or spasticity.
- Reflexes:
| R | L | R | L | ||
| Brachioradialis | 2+ | 2+ | Patellar | 2+ | 2+ |
| Triceps | 2+ | 2+ | Achilles | 2+ | 2+ |
| Biceps | 2+ | 2+ | Babinski | Absent | Absent |
| Abdominal | 2+/2+ | 2+/2+ | Clonus | Negative |
- Meningeal Signs: No nuchal rigidity noted. Brudzinski’s and Kernig’s signs negative
Peripheral Vascular: Skin normal in color and warm to touch upper and lower extremities bilaterally. No calf tenderness bilaterally, no edema present. Pulses are 2+ bilaterally in upper and lower extremities.
Musculoskeletal: Legs restrained by police handcuffs. No edema or erythema noted on bilateral lower extremities without soft tissue swelling, or tenderness. Bilateral shoulder height symmetrical. No obvious deformities.
Assessment:
61-year-old male with a PMH of HTN, T2DM, DCMP, HFrEF, CKD, BPH, bilateral inguinal hernias, pleural effusion, LV thrombus and DVT presents after one syncopal episode in court today.
Differential Diagnosis:
- CHF exacerbation
- Vasovagal syncope
- Orthostatic hypotension
- Arrhythmia
- Stroke
- Pulmonary Embolism
Plan:
#Syncope
- EKG
- CBC, BMP, Troponin, proBNP, d-dimer
- Chest X-ray
- CT head
- CT abdomen-pelvis
- Amlodipine 5mg & Clonidine 0.2mg for hypertensive urgency
- Lovenox 30mg SC q12hr for DVT ppx
- Strict ins and outs, fluid restriction 1L
- Patient refused orthostatics
- Admit to telemetry floor to monitor for arrhythmias and cardiac evaluation with echo
- Plan CTA to r/o PE
- Continue all current home meds
Labs and Imaging:
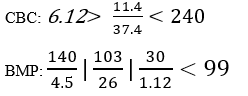
proBNP: 21,903
Troponin: < 0.01
D-dimer: 598
Magnesium: 2.10
EKG: Normal Sinus Rhythm @ 70bpm with non-specific ST changes
CXR: Pulmonary Congestion
CT Head: Small lacunar infarct of indeterminate age right basal ganglia. No acute hemorrhage, hydrocephalus, or infarcts.
CT Abdomen-Pelvis:
- Bilateral inguinal hernias measuring 5.7cm x 3.2cm on the right and 5.4cm x 3.3cm on the left side.
- Post-surgical changes from bilateral hip arthroplasty.
Echocardiogram (12/2021): Mildly increased left ventricular wall thickness
- Grade III left ventricular diastolic dysfunction
- Mildly dilated RV
- Mildly dilated right atrium
- Severely dilated left atrium
- LVEF is 27%
- Cardiology recommended AICD placement in the past but patient has declined


