Identifying Data
June 9th, 2022 – 12:00PM
AT, 66M, Black, Manhattan, NY
Informant: Patient
Chief Complaint: Subacute rehab admission from hospital following above the knee amputation
History of Present Illness:
AT is a 66-year-old male patient who was admitted to Gouverneur SNF for restorative therapy to resume independent ADLs. AT presented to NYU Langone from home on 5/13/22 c/o quickly developing large foot blisters bilaterally, along with a worsening left shin wound. A poor historian and non-compliant with his medication, only reported PMH of T2DM, HTN, and HLD. Prior to hospital presentation, AT lives in a 5th floor walk-up apartment in the Bronx, NY with his wife and two children and is completely independent in all ADLs.
Lab work in the ED revealed a leukocytosis with WBC of 26k and LRINEC (laboratory risk indicator for necrotizing fasciitis) Score of 11 (of 13) and was started on Vancomycin and Zosyn. A right foot x-ray showed gas tracking with overt signs of wet gangrene. His left foot and ankle had multiple bullae along with an unstageable ulcer on his left elbow. On 5/13/22, the vascular team decided to emergently take him to the OR for RLE amputation. A guillotine BKA at the ankle level was attempted but evidence of gray fluid and dead muscle consistent with necrotizing fasciitis present, higher guillotine was performed in the midcalf. After dead muscle was still discovered, patient received right AKA with closure. Pain control achieved with Dilaudid PCA. The glycemic management team was consulted for hyperglycemia and the patient was started on Lantus 15U HS. Additionally, patient was noted to have electrolyte abnormalities with hypernatremia and hypocalcemia along with elevated thyroid function tests, for all of which he was treated.
On 5/15/22, patient developed hypoactive mental status and labs were notable for acute post-op blood loss anemia (H/H 6.5/20.2) and was transfused with 2 units of PRBCs. During this time, patient had a persistent leukocytosis WBC 27k and Clindamycin was added to the standing antibiotic order. Blood cultures returned positive for Streptococcus constellatus.
Dermatology was consulted on 5/15/22 for evaluation of LLE wounds and diagnosed necrotizing small and medium vessel vasculitis. Wound cultures were polymicrobial. Given the findings, rheumatology was consulted on 5/18/22. ABI was 0.5 so a CTA LLE was completed and showed multi-focal femoral artery stenosis.
On 5/20/22, nephrology was also consulted for worsening AKI and electrolyte abnormalities and fluid overload and suggested renal biopsy. TTE was performed and found EF 65%. Chest CT was performed and found multiple hemorrhages, consistent with pulmonary-renal syndrome. On 5/25/22, rheumatology ruled out systemic vasculitis and serial CT-chest showed improvement on opacities with continued antibiotic therapy. The renal biopsy was preformed once that patient was deemed stable on 6/1/22 and revealed infection-associated glomerulonephritis along with glomerulosclerosis, consistent with diabetic nephropathy.
On 6/7/22, labs stabilized, and patient was afebrile and deemed fit for transfer to SAR at Gouverneur for physical therapy and LLE wound care.
Geriatric Assessment:
- ADLs: Completely independent
- IADLs: Completely independent
- Immunizations: Up to date for influenza, COVID-19 with 2 boosters, shingles, and pneumococcal vaccines
- Social Support: Lives with wife and two children
- Urinary incontinence: Fully continent
- Fecal incontinence: Fully continent
- Depression: Screen with PHQ-9 on admission, score of 0. Treatment not recommended
- Advanced Directives: Full code, MOLST on file.
- Health Care Proxy: Wife
Past Medical History:
- T2DM
- HTN
- HLD
- PAD
- Hypothyroidism
Medications:
- Acetaminophen 325mg, 2 tablets PO QID
- Amlodipine 10mg PO QD
- Aspirin 81mg PO QD
- Atorvastatin 10mg PO QD
- Clopidogrel 75mg PO QD
- Gabapentin 200mg PO TID
- Insulin Lispro SS TID before meals
- Janumet (Sitagliptin/Metformin) 50-1000mg PO QD
- Levothyroxine 137mcg PO QD
- Oxycodone 5mg PO prn q6h
- Santyl Ointment 250U/g apply to left lateral calf daily
Allergies:
- NKDA
Family History:
- Mother – alive, unknown medical history, lives in Ghana
- Father – alive, unknown medical history, lives in Ghana
Social History:
AT is a married male, living in the 5th floor walkup in the Bronx, NY with his wife and two children. Prior to hospital admission, he was fully independent on all ADLs. He owns his own convenience store in East Harlem and would like to return to work once he is cleared from the subacute rehab facility. He will require social work involvement upon discharge as there is not an elevator in his building. He is open to the idea of a prosthetic leg if he is able to afford one. Since his hospitalization, AT has become spiritual, stating that God is the only reason that he is alive and would like religion to be a part of his care.
- Diet: Does not follow specific diet regimen, his wife does the cooking at home.
- Smoking: Denies current or previous use of all tobacco products
- Alcohol: Denies current or previous use of alcohol
- Drugs: Denies current or previous use of any illicit drugs.
- Exercise: Unable to exercise following amputation. Patient admits that walking was his exercise prior to procedure. Admitted for rehabilitation, will be receiving PT daily.
- Safety Measures: Patient currently cleared to ambulated to restroom using rolling walker.
- Sexual History: Not currently sexually active. Has two children. Denies history of STIs.
- Occupational History: Patient owns his own convenience store in East Harlem since 1996
Review of Systems:
General: Denies any recent weight loss or gain, or loss of appetite. Denies night sweats, fever, or chills.
Skin, hair, and nails: Admits to excessive dryness and discoloration of left lower extremity, site of multiple arterial wounds. Otherwise, denies changes in texture, excessive dryness or sweating, changes in pigmentations, moles/rashes, pruritus, or changes in hair distribution.
Head: Denies headaches, migraines, vertigo, nausea, or vomiting.
Eyes: Denies use of glasses or other corrected vision. Denies visual disturbances, excess tearing or dryness, photophobia, or pruritis. Last eye exam 3 years ago.
Ears: Denies hearing loss, tinnitus, vertigo, discharge, earache.
Nose and sinuses: Denies discharge, obstruction, or epistaxis
Mouth and throat: Denies sore throat or trouble swallowing. Denies bleeding gums, ulcerations. Does not wear dentures. Last dental exam 3 years ago.
Neck: Denies localized swelling, lumps, stiffness, or decreased range of motion.
Pulmonary: Denies shortness of breath, cough, wheezing, hemoptysis, cyanosis, orthopnea, or paroxysmal nocturnal dyspnea.
Cardiovascular: Denies chest pain, irregular rhythms, or palpitations. Admits to ulceration on left lower extremity.
Gastrointestinal: Has no change in bowel habits, with no changes in color or consistency. Denies changes in appetite, intolerance to any foods, no nausea/vomiting/dysphagia, pyrosis. No constipation, bleeding, (hemorrhoids, melena, or hematochezia), or abdominal pain. Has never had a colonoscopy.
Genitourinary: Denies incontinence. Denies dysuria, nocturia, oliguria, or polyuria.
Nervous: Denies history of seizures Denies headache, loss of consciousness, sensory disturbances, or change in cognition/mental status/memory.
Musculoskeletal: Denies joint pain or limited range of motion.
Peripheral Vascular: Admits lower extremity ulcers.
Hematologic: Denies history of DVT, has history of receiving blood transfusion.
Endocrine: Denies heat/cold intolerance, excessive sweating.
Psychiatric: Denies history of depression and anxiety. Denies having SI/HI or previously seeing a mental health professional.
Physical Exam:
General: 66M, A&O x3, lying on bed dressed, speaking in full sentences, not in acute distress. He is well groomed and well-developed for age. Not cachectic.
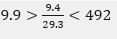
Vitals:
- BP(Sitting): L – 128/89 mmHg
- P: 90 regular
- R: 14breaths/min, unlabored
- T: 98.0F (36.7C), oral
- O2 Sat: 99% on room air
- Blood sugar: 97
- Height: 68inches – Weight: 149.1lbs – BMI: 22.7 (Healthy)
Skin: Poor turgor throughout, non-icteric. AKA, right leg. Added to report for wound care team to evaluate the following:
- 2.9cm x1.8cm unstageable ulcer, left elbow, covered by occlusive dressing
- 2.6cm x5.0cm blister, left dorsum foot
- 5.0cm x 3.2cm blister, left lateral malleolus
- 9.0cm x 3.9cm venous ulcer, left calf
Hair: Low, evenly distributed. No alopecia, nits, or seborrhea noted
Nails: Capillary refill <2 seconds in all three extremities. In-house podiatry and wound care consulted on 6/9/22.
Head: Normocephalic. No visible trauma.
Eyes: Symmetrical OU. No strabismus, exophthalmos, sclera white, cornea clear, conjunctiva pink.
- Vision uncorrected – 20/30 OS, 20/40 OD, 20/30 OU
- Visual fields full OU. PERRLA, EOMs intact with no nystagmus
- Fundoscopy – Red reflex intact OD only. No AV nicking, hemorrhages, or exudates lens problem
- Visual fields diminished OU. PERRLA, EOMs intact with no nystagmus
Ears: Symmetrical and appropriate in size. No masses, lesions, or deformities on external ears. No discharge or foreign bodies in external auditory canals AU. TM’s white and intact with light reflex in good position AU.
Mouth:
- Lips: Pink and moist with no lesions
- Mucosa: Pink with no masses or lesions. Well hydrated. No leukoplakia.
- Palate: Pink, well hydrated.
- Teeth: Fair dentition, no missing teeth, does not wear dentures.
- Gingivae: Pink. No hyperplasia; masses; lesions; erythema or discharge.
- Tongue: Pink; well papillated with no masses or lesions.
- Oropharynx: Well hydrated, no masses, lesions, or foreign bodies. Uvula pink, no edema
Neck: Trachea midline. 2+ Carotid pulses, no stridor, thrills, or bruits noted bilaterally.
Thyroid: Nontender to palpation, no masses, no bruits noted. No thyromegaly.
Chest: Symmetrical, no deformities or trauma. Respirations unlabored, no paradoxical respirations or use of accessory muscles noted. Non-tender to palpation throughout.
Lungs: No wheezing, rhonchi, or rales. Chest expansion symmetrical. Tactile fremitus symmetric throughout.
Heart: Carotid pulses are 2+ bilaterally without bruits. RRR, S1 and S2 are distinct with no murmurs, S3 or S4. PMI in 5th ICS in mid-clavicular line.
Abdomen: Abdomen is symmetric with striae, no pulsations. Bowel sounds normoactive in all four quadrants with no aortic/renal/iliac/femoral bruits. Non-tender to light or deep palpation. Tympanic throughout, no hepatosplenomegaly to palpation, liver span approximately 7cm. No CVA tenderness appreciated
Neurologic:
- Mental Status: Alert and oriented to person, place, time, and situation. Receptive and expressive abilities intact. Thought coherent, no dysarthria, dysphonia, or aphasia. Memory and attention intact.
- CN I: Correctly identifies alcohol swab and an orange.
- CN II: No loss of visual fields peripherally in all 4 quadrants OU. Refer to eye portion of PE for fundoscopy & visual acuity.
- CN III, IV & VI: EOMs intact with no nystagmus, pupils 3 mm OU and reactive to direct and consensual light. No red reflex OS.
- CN V: Face sensation symmetrical and intact bilaterally. Jaw strength intact.
- CN VII: Facial expressions intact, clearly enunciates words. Did not test: sweet, salt and sour tastes.
- CN VIII: Repeats whispered words at 2 feet bilaterally, Weber – no lateralization, Rinne – AC>BC AU
- CN IX & X: No hoarseness, uvula midline with elevation of soft palate. No pain noted while swallowing. Gag reflex intact.
- CN XI: full range of motion at neck with 5/5 strength and good shoulder shrug
- Motor/Cerebellar: Patient currently weight-bearing with assistance of rolling walker. Completes physical therapy 5x/week for 1 hour per session. Full active ROM in upper extremities, weak active ROM in left lower extremity but without rigidity or spasticity.
- Sensory: Intact to light touch, sharp/dull, and vibratory sense throughout. Proprioception, point localization, extinction, stereognosis, and graphesthesia intact bilaterally.
Reflexes:
| R | L | R | L | ||
| Brachioradialis | 2+ | 2+ | Patellar | Unable | 2+ |
| Triceps | 2+ | 2+ | Achilles | Unable | 2+ |
| Biceps | 2+ | 2+ | Babinski | Unable | Absent |
| Abdominal | 2+/2+ | 2+/2+ | Clonus | Negative |
Peripheral Vascular: Skin normal in color and warm to touch upper extremities bilaterally. Patient does express left calf tenderness without edema. Pulses are 2+ bilaterally in upper and left lower extremities. Patient has multiple left lower extremities injuries secondary to PAD, outlined in skin exam.
Musculoskeletal: No edema but erythema present on LLE. Tenderness appreciated left calf, currently wrapped in Kerlix. Bilateral shoulder height symmetrical.
Recent Labs:
CBC:
BMP:
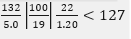
HgbA1c: 8.5%
TSH: 5.94
Assessment and Plan:
#PAD
- Currently stable s/p right AKA with closure (5/13) and angiogram with angioplasty of left SFA and popliteal artery (5/20)
- Continue Tylenol 650mg PO QID
- Continue Oxycodone 5mg PO q6h prn, wean as tolerated
- Continue gabapentin 200mg PO TID
- Continue daily dressing changes to LLE. Clean with sterile salize moistened gauze, apply thin film of Bacitracin ointment, apply Dakins’ moistened wet-to-dry gauze over left later calf lesions, cover with dry gauze, wrap entire left calf with Kerlix.
- Clean right AKA site daily with soap/water, leaving retention sutures in place.
- Continue with daily PT, 1hour/day.
- Follow-up appointment with vascular surgeon on 6/24/22.
#HTN/HLD
- Currently stable
- Continue Plavix 75mg PO QD
- Continue Amlodipine 10mg PO QD
- Continue Atorvastatin 10mg PO QD
- Monitor v/s
#T2DM
- HgbA1c 8.5%
- Continue lispro low dose SS TID
- Janumet (Sitagliptin/Metformin) 50-1000mg PO QD
#Hypothyroidism
- Synthroid 137mcg PO AM, 30 minutes prior to other meds
- Repeat TSH/Free T4 in 4-6 weeks
#Discharge Plan
- Upon discharge, social work to work with family regarding living in a 5th floor walkup with no elevator


