Identifying Data
September 6th, 2022 – 7:45
HS, 8F, Hispanic, Queens, NY
Informant: Parent through Spanish interpreter
Referral Source: Self
Chief Complaint: Abdominal pain
History of Present Illness:
8-year-old female with a past medical history of constipation and UTI presents to the ED with her father complaining of abdominal pain since yesterday. The pain is generalized, worse with urinating, rated a 7 out of 10, and described as burning. The patient has had one normal bowel movement in the past 24 hours where she had to push. She admitted to having rice for dinner last night and cereal for breakfast this morning, both without difficulty. Father denies giving her any medications for the pain. There are no aggravating factors. She was treated for constipation and a UTI in December 2021 without complications. Father denies sick contacts at home, school, or recent travel. Denies fever, chills, chest pain, shortness of breath, nausea, vomiting, diarrhea, dizziness, lightheadedness, headache, back pain, rhinorrhea, or sore throat.
Past Medical History:
- Constipation
- UTI
Past Surgical History: Denies
Medications: Denies
Allergies: Denies
Vaccinations: Up to date
Family History:
- Mother – 36, alive and well, no known medical conditions
- Father – 37, alive and well, no known medical conditions
- Sister 1 – 14, no known medical conditions
- Sister 2- 10, no known medical conditions
Social History:
- Home: Lives at home with parents, and two sisters
- Occupation: 4th grade student
- Smoking: Denies
- Alcohol: Denies
- Drugs: Denies
- Sleep: Sleeps 9 hours per night
- Travel: No recent travel or sick contacts
Review of Systems:
General: Denies any recent weight loss or gain, loss of appetite, generalized weakness or fatigue, night sweats, fever, or chills
Skin, hair, and nails: Denies changes in texture, excessive dryness or sweating, discolorations, pigmentations, moles/rashes, pruritus, or changes in hair distribution.
Head: Denies headaches, migraines, vertigo, nausea, or vomiting.
Eyes: Positive corrected vision. Denies blurry vision, photophobia, double vision, excess tearing, dryness, or pruritis. Last eye exam in June 2022.
Ears: Denies hearing loss, tinnitus, vertigo, discharge, earache.
Nose and sinuses: Denies discharge, obstruction, allergies, or epistaxis
Mouth and throat: Denies sore throat. Denies bleeding gums, ulcerations. Last dental exam in May 2022.
Neck: Denies stiffness, decreased range of motion, localized swelling, or lumps.
Pulmonary: Denies shortness of breath, wheezing, or productive cough. Denies hemoptysis, cyanosis, orthopnea, or paroxysmal nocturnal dyspnea.
Cardiovascular: Denies chest pain, palpitations, edema, irregular rhythms.
Gastrointestinal: Positive for abdominal pain. Has no change in bowel habits, with no changes in color or consistency. Denies changes in appetite, intolerance to any foods, no nausea/vomiting/dysphagia, pyrosis, or bleeding (hemorrhoids, melena, or hematochezia).
Genitourinary: Positive for dysuria. Denies incontinence, nocturia, urgency, oliguria, or polyuria.
Nervous: Denies headaches, seizures, loss of consciousness, sensory disturbances, ataxia, loss of strength, change in cognition/mental status/memory, or weakness.
Musculoskeletal: Denies joint pain, swelling, weakness, and changes in range of motion.
Peripheral Vascular: Denies peripheral edema. Denies intermittent claudication.
Hematologic: Denies history of DVT/PE or previous blood transfusions.
Endocrine: Denies heat/cold intolerance, excessive sweating.
Psychiatric: Denies history of depression and anxiety. Denies having SI/HI or previously seeing a mental health professional.
Physical Exam:
General: 8F, A&O x3, walking around in no acute distress. She is well groomed and well-developed for age. She does not appear ill.
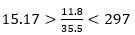
Vitals:
- BP(Seated): R – 106/72
- P: 107, regular
- R: 18breaths/min, unlabored
- T: 99.1F (37.3C), oral
- O2 Sat: 99% on room air
- Height: 49 inches – Weight: 72lbs – BMI: 21.1 – Overweight
Skin: Warm and moist with good turgor throughout. Nonicteric. No lower extremity erythema and warmth. Nontender on palpation. No cyanosis or jaundice.
Hair: Average quantity and distribution.
Nails: No clubbing, capillary refill <2 seconds in all four extremities
Head: Normocephalic, atraumatic, nontender to palpation throughout.
Eyes: Symmetrical OU. No strabismus, exophthalmos, sclera white, cornea clear, conjunctiva pink.
- Visual corrected – 20/20 OS, 20/20 OD, 20/20 OU from 6feet with pocket Snellen
- Visual fields full OU. PERRLA, EOMs intact with no nystagmus
- Fundoscopy – Red reflex intact OU. Cup to disk ratio< 0.5 OU. No AV nicking, hemorrhages, or exudates
Ears: Symmetrical and appropriate in size. No masses, lesions, or deformities on external ears. No discharge or foreign bodies in external auditory canals AU. TM’s white and intact with light reflex in good position AU.
Mouth:
- Lips: Pink and moist with no lesions
- Mucosa: Pink with no masses or lesions. Non-tender to palpation. No leukoplakia.
- Palate: Intact with no masses or lesions Non-tender to palpation; continuity intact.
- Teeth: Good dentition with no obvious dental caries noted.
- Gingivae: Pink. No hyperplasia; masses; lesions; erythema or discharge.
- Tongue: Pink; well papillated with no masses or lesions. Non-tender to palpation.
- Oropharynx: Well hydrated, no masses, lesions, or foreign bodies. Grade 1 tonsils, class II Mallampati score. Uvula pink, no edema
Neck: Trachea midline. 2+ Carotid pulses, no stridor, thrills, or bruits noted bilaterally.
Thyroid: Nontender to palpation, no masses, no bruits noted. No thyromegaly.
Chest: Symmetrical, no deformities or trauma. Respirations unlabored, no paradoxical respirations or use of accessory muscles noted. Non-tender to palpation throughout.
Lungs: Clear to auscultation and percussion bilaterally. Chest expansion and diaphragmatic excursion symmetrical. Tactile fremitus symmetric throughout. No adventitious sounds.
Heart: Carotid pulses are 2+ bilaterally without bruits. RRR, S1 and S2 are distinct with no murmurs, S3 or S4. PMI in 5th ICS in mid-clavicular line.
Abdomen: Abdomen is symmetric without striae, no pulsations. Bowel sounds normoactive in all four quadrants with no aortic/renal/iliac/femoral bruits. There is generalized tenderness to light and deep palpation, most significant in the right lower quadrant with guarding and rebound tenderness. No CVA tenderness appreciated.
- McBurney’s sign: Negative
- Rovsing’s sign: Negative
- Obturator sign: Negative
- Iliopsoas sign: Negative
Neurologic:
- Mental Status: Alert and oriented to person, place, and time. Receptive and expressive abilities intact. Thought coherent, no dysarthria, dysphonia, or aphasia. Memory and attention intact.
- CN II-XII grossly intact.
- Motor/Cerebellar: Full active ROM of all extremities without rigidity or spasticity. No atrophy, tics, tremors, or fasciculation.
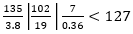
- Reflexes:
| R | L | R | L | ||
| Brachioradialis | 2+ | 2+ | Patellar | 2+ | 2+ |
| Triceps | 2+ | 2+ | Achilles | 2+ | 2+ |
| Biceps | 2+ | 2+ | Babinski | Absent | Absent |
| Abdominal | 2+/2+ | 2+/2+ | Clonus | Negative |
- Meningeal Signs: No nuchal rigidity noted. Brudzinski’s and Kernig’s signs negative
Peripheral Vascular: Skin normal in color and warm to touch upper and lower extremities bilaterally. No calf tenderness bilaterally, no edema present. Pulses are 2+ bilaterally in upper and lower extremities.
Musculoskeletal: No edema or erythema present on bilateral upper and lower extremities without soft tissue swelling, or tenderness. Full active ROM of all extremities. Bilateral shoulder height symmetrical. No obvious deformities. Strength 5/5 in both upper and lower extremities. Grip 5/5 bilaterally.
Assessment:
8-year-old girl with generalized abdominal pain, greatest in the right lower quadrant.
Differential Diagnosis:
- Appendicitis
- Constipation
- UTI
Plan:
#Abdominal pain
- CBC:
- CMP:
- Calcium: 9.6
- Alk Phos: 296
- ALT: 14
- AST: 23
- UA: + for trace blood and occasional bacteria
- Type & Screen: O+
- NPO
- Acute abdomen series
- Bowel gas pattern is mildly distended but nonobstructive
- Moderate stool burden
- Acetaminophen 15mg/kg PO (500mg) given
- Patient transferred to Bellevue for ultrasound of the appendix
Post-Transfer Follow-Up:
- US abdomen
- US abdomen with no normal or abnormal appendix able to be identified.
- Surgery consulted
- MRI abdomen and pelvis ordered
- MRI Abdomen/Pelvis
- Acute appendicitis. No abscess
- Laparoscopic appendectomy
- Completed 9/7/22 11:45


